The information in this article comes from: "Chinese Journal of Dermatology"
Psoriasis in children is a chronic disease that occurs in children (age < 18 years old) and is induced by a combination of genetic and environmental factors (such as infection, etc.) Recurrent, immune, and systemic skin diseases. The clinical manifestations of psoriasis in children are complex and the types vary greatly. Due to the special physiological characteristics of children, safety should be paid more attention to in treatment. Compared with adults, the treatment of psoriasis in children is more limited and challenging. For example, the ideal therapeutic dose of systemic drugs, the adverse effects of long-term treatment, the choice of combination drugs, and the conversion of drugs have not yet been clarified. Many drugs, including topical and systemic drugs, are not approved for the treatment of psoriasis in children. The purpose of establishing a consensus on the diagnosis and treatment of psoriasis in children is to more effectively and scientifically standardize the diagnosis and treatment of psoriasis in children, to guide physicians to control the occurrence and development of psoriasis in children in a timely and effective manner, to improve and enhance the quality of life of children and their families, and to help patients The child develops and grows as healthy as possible.
Expert consensus on diagnosis and treatment of psoriasis in children in China (2021)
Psoriasis Group, Dermatology Branch of Chinese Medical Association
Pediatrics Group, Chinese Medical Association Dermatology Branch
Corresponding author: Zhang Xibao, Email: zxibao@126.com; Ma Lin, Email: bch_maleen@aliyun.com; Zhang Xuejun, Email: ayzxj@vip.sina.com
[Cite this article] Psoriasis Group of Chinese Medical Association Dermatovenereology Branch, Pediatrics Group of Chinese Medical Association Dermatovenereology Branch. Expert consensus on diagnosis and treatment of psoriasis in children in China (2021) [J]. Chinese Journal of Dermatology, 2021, 54 (7): 559-581. doi: 10.35541/cjd.20201065
[Keywords] Psoriasis; children; diagnosis; treatment; guidelines for diagnosis and treatment
1. Current status of diagnosis and treatment and existing problems At present, the diagnosis of psoriasis in children in China is often based on clinical manifestations. Psoriasis in younger infants and young children mostly occurs in the diaper area. The clinical manifestations are lacking and the diagnosis is quite difficult. . The common type of psoriasis in older children is plaque psoriasis (75%). Compared with adults, the erythema covered with white scales is smaller and thinner, and the infiltration is not obvious. It often occurs on the flexion side of the face and body. ; Followed by guttate psoriasis (15% ~ 30%), generalized pustular psoriasis (GPP) (1% ~ 5.4%), psoriatic arthritis in children accounted for juvenile idiopathic arthritis In 5% of patients, palmoplantar pustular psoriasis, reverse psoriasis, and erythroderma psoriasis are rare. The disease can affect special parts such as nails and scalp.
The principle of psoriasis treatment in children is the same as that in adults, and corresponding treatments are given for different causes, types and stages of disease. Pay attention to the psychological treatment of guardians and older children to avoid inducing or aggravating factors such as infection and fatigue. Due to the long-term effects of comorbidities and chronic and recurrent characteristics of psoriasis in children, more attention is paid to active treatment and life-long management. Most children with psoriasis are mild and usually only require topical medication. Phototherapy can also be performed when necessary, and a small number of moderate to severe children require systemic drug treatment. In recent years, small-molecule targeted drugs and biological agents [tumor necrosis factor alpha (TNF-α) inhibitors, interleukin (IL)-12/IL-23 inhibitors and IL-17 inhibitors] have also been gradually approved in different countries It is used for the treatment of psoriasis in children, and has shown a good effect.Due to the special physiological characteristics of children, more attention should be paid to the safety of treatment, and the ideal therapeutic dose of systemic drugs, long-term adverse effects, the choice of drug combination, and the conversion of drugs should also be considered. The clear treatment guidelines for adults are not applicable to children. Many drugs, including topical drugs and systemic drugs, are not approved for this age. At present, most treatments for psoriasis in children are based on expert consensus and experience. There are few clinical trial data on the efficacy and toxicity of systemic drugs in the treatment of psoriasis in children, and there is no standardized treatment plan at home or abroad.Two, etiology and pathogenesis Similar to adults, the etiology and pathogenesis of psoriasis in children have not been fully elucidated. Genetic background (family history, HLA-Cw6 susceptibility alleles, IL-36 receptor antagonist deletion and CARD14 gene mutation, etc.), environmental triggers (pharyngeal and perianal hemolytic streptococcal infection, smoking, physical and psychological Stress, trauma and certain drugs, hormone withdrawal, obesity), abnormal immune response (interaction between immune cells, overexpression of cytokines) and other factors interact, eventually leading to the occurrence of psoriasis.
Three. Epidemiology
Different countries report the prevalence of psoriasis in children under 18 years of age from 0.7% to 1.2%, and the prevalence of psoriasis in Chinese children from 10 to 19 years old is 0.18 %. Compared with other races, Caucasian children have a higher prevalence and an earlier average age of onset. There is also a certain relationship between latitude and prevalence. The farther from the equator, the higher the prevalence. Family history of psoriasis in children has been widely reported. About 30% of first-degree relatives of children with psoriasis suffer from psoriasis.
Four. Clinical manifestations and classification
According to the clinical manifestations, psoriasis in children is divided into vulgaris, pustular, erythroderma and arthropathy. Psoriasis vulgaris is the most common type of psoriasis in children. According to the clinical manifestations, it can be divided into plaque psoriasis and guttate psoriasis. 1. Plaque psoriasis: accounts for about 70% of psoriasis in children. Compared with adults, the erythema covered with white scales is smaller and thinner. The infiltration is not obvious and often occurs on the flexion side of the face and body surface. The scalp is usually the first site of psoriasis in children, and it is more likely to occur in girls. Reverse psoriasis is more common in children than adults. Psoriasis in the diaper area is a special type of psoriasis in children. It is common in infants < 2 years old. It is different from diaper dermatitis. Psoriasis in the diaper area has clear boundaries. It is characterized by bright red and slightly raised plaques, often accompanied by maceration, and the groin area is often affected. 2. guttate psoriasis: often acute onset, there is often a history of upper respiratory tract infection caused by hemolytic streptococcus 1 to 3 weeks before the rash. The clinical manifestations are clear red papules and maculopapular rashes with a diameter of 1-10 mm, covered with a little scaly. The trunk and proximal extremities are the most common, with varying degrees of itching. Guttate psoriasis has a tendency to subside spontaneously, and some continue to develop into plaque psoriasis. Recurrent pustular psoriasis in childhood is an autoinflammatory oligogenetic genetic disease. The most common mutant genes are IL-36RN, CARD14, Other related genes reported are AP1S3, SERPINA3 and MPO, which are clinically divided into two types: generalized pustular psoriasis (GPP) and localized pustular psoriasis. Among them, GPP in children includes acute GPP, pustular psoriasis in children, pustular psoriasis in infants and young children, and limited types of GPP; localized pustular psoriasis in children includes palmoplantar pustulosis and continuous limbs. End dermatitis.(3) Erythroderma-type psoriasis
This type of child is rare, often due to psoriasis stimulated by certain factors or improper treatment induced, pustular psoriasis can also be in the process of pustular regression Behave as this type. The clinical manifestations are diffuse flushing, infiltration and swelling of the skin all over the body, accompanied by a large number of bran-like scales, during which normal skin islands can be seen, often accompanied by systemic symptoms such as fever and chills.(4) Psoriasis of joint disease
Also known as psoriasis arthritis (psoriasis arthritis, PsA), most PsA secondary to psoriasis, a small part of arthritis and psoriasis at the same time Occurs or precedes psoriasis. PsA can start at any age in children, and the peak is 2 to 3 years old (early onset) and 10 to 12 years old (late onset). The clinical manifestations are mainly inflammatory arthritis. Early-onset children with PsA are more common in girls and often manifest as dactylitis, oligoarthritis or polyarthritis. Late-onset PsA is more common in boys, HLA-B27 positive rate is high, and axial involvement is more common than early-onset PsA.
Five. Comorbidity of psoriasis
Psoriasis children with hyperlipidemia, obesity, high blood pressure, diabetes and rheumatoid arthritis increased twice the risk, Crohn's disease The rate is 4 times higher, and asthma may also be one of the comorbidities of psoriasis in children. Co-morbidities of psoriasis in children include obesity, metabolic syndrome in children and adolescents, cardiovascular disease, and mental and emotional disorders.
VI. Diagnosis and differential diagnosis
Based on the characteristics of the skin lesions, combined with medical history data, including the first involved site, accompanying symptoms, previous infection history, history of vaccination, physical and psychological trauma, and past medical history (Type 1 diabetes, Crohn’s disease, mental illness), etc. for diagnosis. Typical signs (wax drop phenomenon, thin film phenomenon, spotting hemorrhage) have diagnostic value. For atypical skin lesions, imaging techniques such as dermoscopy, reflective confocal microscope, skin ultrasound can help diagnose, and skin tissue pathology is important for diagnosis. value. Psoriasis in children needs to be differentiated from atopic dermatitis, nummular eczema, tinea corporis, pityriasis red, lichen planus, and chronic pityriasis lichenoides.
Seven. Treatment
The treatment of psoriasis in children includes topical drugs, phototherapy, systemic drugs, etc., and other adjuvant treatments include antibiotics and tonsillectomy. In addition to considering the child’s age, disease type, severity and impact on the quality of life when choosing a treatment plan, due to the child’s special physiological characteristics, more attention should be paid to the safety of treatment. Patient education and psychological support are also important parts of treatment.
(1) External medication treatment
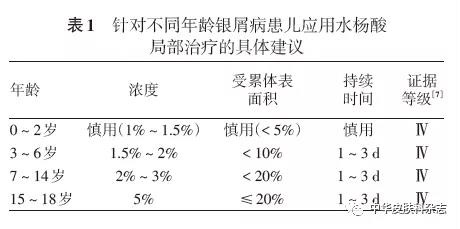
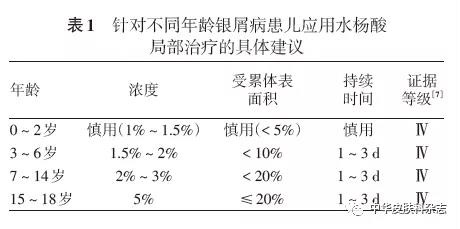
Topical drug therapy is the first-line treatment option for psoriasis in children, including hormones, vitamin D3 derivatives (such as calcipotriol), and calcineurin inhibitors (Tacrolimus and pimecrolimus), tretinoin preparations (commonly used 0.05% and 0.1% tazarotene preparations), keratolytic agents (commonly used lactic acid, simethicone, salicylic acid, high-concentration urea Ointment), others (keratin promoter, anti-human IL-8 monoclonal antibody cream, benvimod cream, Janus kinase inhibitor, phosphodiesterase 4 inhibitor, anthralin, etc.). Among them, topical hormones are the most commonly used drugs for the treatment of psoriasis. Avoid sudden discontinuation after the skin lesions are basically controlled. A reduction or weekend treatment mode should be adopted to extend the remission time; in order to improve the safety of topical topical hormones for long-term use and reduce adverse reactions , Hormonal and non-hormonal topical drugs can be used in combination or sequential treatment.
Ultraviolet rays clinically used in the treatment of psoriasis in children include narrow-band mid-wave ultraviolet (NB-UVB) and long-wave ultraviolet (mainly PUVA, including external and oral supplements). Bone fat + UVA) and 308 excimer light/laser. Among them, NB-UVB (311 ~ 313 nm) is currently the main phototherapy method for the treatment of psoriasis. Its safety is better than PUVA. It is suitable for moderate to severe stubborn psoriasis and plaque psoriasis in children. Children younger than 10 years old should be cautious. Use; 308 excimer light/laser is suitable for mild to moderate stable stage localized plaque psoriasis and facial psoriasis, and can also be used for folds and palms, plantars, knees, elbows, scalp and other refractory parts, Skin lesion area is generally<10% BSA; PUVA is contraindicated in children under 12 years old, topical psoralen + UVA is suitable for localized plaque psoriasis, and those who are ineffective or contraindicated to NB-UVB and other system treatments .(3) Systemic drug therapy
For moderate to severe psoriasis that progresses quickly or has complications that may affect the quality of life of the child, external medication or phototherapy cannot effectively control the disease, need to be evaluated Do you need systemic treatment? Systemic drug treatment of psoriasis in children includes methotrexate, tretinoin (Acitretin), cyclosporine, biological agents (such as TNF-α inhibitor etanercept, infliximab, adalimumab) Anti-IL-12/IL-23 inhibitor Uselnumumab, IL-23 inhibitor Gusezumab, IL-17 inhibitor Skucilizumab, Ichizumab), other systemic Drugs (fumarate, etc.). Methotrexate is currently the most common systemic drug for the treatment of moderate to severe psoriasis in children. It is effective for all types of psoriasis, including moderate to severe plaque, arthropathy, erythroderma, psoriasis, and pustular psoriasis. Psoriasis has definite curative effect, and the level of evidence is Ⅱ~Ⅲ, but there is still no recognized standardized treatment plan for psoriasis in children. Acitretin can be used to treat generalized guttate or moderate to severe plaque psoriasis or pustular psoriasis in children. It is recommended that acitretin A is started in sufficient quantity and slowly stopped. The few studies suggest that cyclosporine has a certain effect in the treatment of children with multiple/few joint juvenile idiopathic arthritis and psoriatic juvenile idiopathic arthritis.8. Disease prevention and health education Disease prevention is mainly reflected in several aspects: ①Skin care, including basic skin care (using emollients) and removing scales (using keratolytic agents) ); ②Prevention of colds and other infections, including vaccination of common vaccines, inactivated vaccines, live vaccines and prevention of infection exposure; ③Diet recommendations, low-tryptophan diet and reducing the consumption of red meat, high-fat foods, etc., appropriate amount Supplementing omega-3 fatty acids (fish oil), vitamin D, vitamin B12, and selenium may be beneficial to children with psoriasis; ④Skin care recommendations, regular use of emollients or moisturizers is very important for children with psoriasis.
Health education can increase patients and guardians' understanding of diseases, develop good skin care habits, avoid irritation and inducing factors, and improve treatment compliance. Psychotherapy is also an indispensable part of the treatment of psoriasis, helping children build self-confidence and treat the disease correctly.
Experts who participated in the development of this consensus (sorted by pinyin of their names)
Chen Hongxiang (Xinhua Hospital Affiliated to Tongji Medical College of Huazhong University of Science and Technology), Cui Yong (China-Japan Friendship Hospital), Geng Songmei (Second Affiliated Hospital of Xi'an Jiaotong University), Li Ming (Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine), Li Ping (Shenzhen) Municipal Children’s Hospital), Li Yuzhen (The Second Affiliated Hospital of Harbin Medical University), Liang Yanhua (Shenzhen Hospital of Southern Medical University), Ma Lin (Beijing Children’s Hospital of Capital Medical University), Qian Qiufang (Shanghai Children’s Hospital), Ren Yunqing (Zhejiang University Medicine Children’s Hospital Affiliated to the Hospital), Shi Yuling (Shanghai Dermatology Hospital), Shu Hong (Kunming Children’s Hospital), Tang Jianping (Hunan Children’s Hospital), Wang Hua (Children’s Hospital of Chongqing Medical University), Wang Liuhui (Pediatrics Department of Fudan University) Hospital), Xu Zigang (Beijing Children's Hospital Affiliated to Capital Medical University), Zeng Huasong (Guangzhou Women and Children's Medical Center), Zhang Chunlei (Peking University Third Hospital), Zhang Xibao (Institute of Dermatology, Guangzhou Medical University), Zhang Xuejun (Suzhou University Shuhu Hospital), Zheng Min (The Second Affiliated Hospital of Zhejiang University School of Medicine), Zhu Wu (Xiangya Hospital of Central South University)
Writing Secretary: Zhang Sanquan (Guangzhou Institute of Dermatology), Zhu Zhengwei (The First Affiliated Hospital of Anhui Medical University)
References (omitted, those interested can go to the official website of this journal to view)
Copyright statement: The information in this article comes from: "Chinese Journal of Dermatology"